Abstract
MYC amplification (amp) is a marker of poor prognosis in many non-hematologic malignancies. While MYC translocations in B cell lymphoma (BCL) have been extensively studied, little is known about the significance of MYC amp. Recent studies describe increased MYC copy numbers (3-10 copies/cell) to be associated with more aggressive BCL. The WHO 2017 does not include MYC amp in the definition of high-grade BCL (HGBCL) with MYC and BCL2 and/or BCL6 rearrangement ("double-hit lymphoma", DHL). However, it also states that high-level MYC amp occurring together with a MYC rearrangement, and concurrent with BCL2 rearrangement likely has a similar clinical impact as classic DHL. Although increased MYC copy number is commonly identified by routine fluorescence in situ hybridization (FISH) testing in BCL, the experience of our large cytogenetics reference laboratory suggests that high-level MYC amp, defined as uncountable MYC signals, is far less common. Therefore, we sought to characterize the clinical, pathologic and cytogenetic features of patients with BCL showing high-level MYC amp.
The Mayo Clinic cytogenetic database was retrospectively reviewed for all cases of BCL with high-level MYC amp seen by FISH from January 2010 - February 2018. All FISH studies reported as MYC amp were re-reviewed by a cytogeneticist to verify the level of amp and the MYC probes involved. Pathology was reviewed by two independent hematopathologists. Clinical information was collected through chart review. Survival analysis was performed using Kaplan-Meier curves and the Wilcoxon rank-sum test.
FISH analysis for MYC aberrations identified 44/9715 (0.45%) cases with high-level MYC amp. Of cases with available H&E, the most common morphology was diffuse large BCL (DLBCL) (82%; 28/34), followed by HGBCL (15%; 5/34) and plasmablastic BCL (3%; 1/34). Hans cell of origin (COO) algorithm immunohistochemistry (IHC) identified 21/25 (84%) germinal center B-cell-like (GCB), and 4/25 (16%) non-GCB cases. 21/27 (78%) cases were BCL2+ by IHC. MYC+ by IHC was ≥40% in 21/28 (75%) and <40% in 7/28 (25%) cases. 9/17 (53%) were "double expressers" (DEL) by IHC.
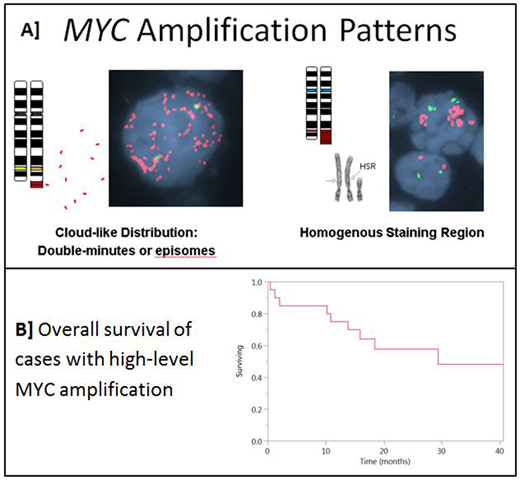
MYC amp probe signals appeared in a cloud-like distribution (CLD) in 31 (70%) or in a single homogenous staining region (HSR) in 13 (30%) [Figure 1A]. Among 38 cases with amp in a MYC break-apart probe, 21 (55%) had amp of 5' alone, 15 (40%) of intact and 2 (5%) of the 3' probe alone. 7/44 (16%) had MYC translocations (5 IGH; 2 non-IGH). BCL2 rearrangement was seen in 15/39 (38%) cases, and BCL6 rearrangement in 3/36 (8%). Only 2/44 (4%) cases met the current WHO 2017 definition of DHL.
Clinical data was available for 20 cases. Median age at diagnosis was 64.5 (range 25-88) years with M:F of 1.5:1. Only 1/14 (7%) had bone marrow while 16/18 (88.8%) had other extranodal sites of involvement (8 gastrointestinal). The clinical presentation was heterogeneous: 13 de novo, 3 post-transplant, 3 transformed from low grade and 1 mediastinal BCL. 9/14 had an elevated LDH, median 387 (225 - 2063) U/L. R-CHOP was the most common first line therapy in 12/17 (70%). At median follow-up of 18.2 (range 0.4 - 88.9) months, 9 patients had died, 3 were in relapse and 8 remained in first complete remission. Lymphoma relapse/progression was the most common cause of death in 7/9 (78%). The median overall survival (OS) was 29.3 months [Figure 1B]. There was no statistically significant difference in OS by morphologic classification (DLBCL vs HGBCL, p=0.6), double expresser (Yes/No, p=0.19), COO (GCB vs non-GCB, p=0.08), MYC amp pattern (HSR vs CLD, p=0.48), MYC amp probe (3' vs 5' vs intact, p=0.31), MYC rearrangement (Yes/No, p=0.1), or MYC amp with concurrent BCL2/BCL6 rearrangement (Yes/No ,p=0.2).
To our knowledge, this is the first study to characterize the clinical, pathologic and cytogenetic features of BCL with strictly-defined high level MYC amp identified by FISH. The 5' signal alone, or the intact MYC probe are most frequently amplified, and two distinct patterns of amp can be seen. Predominant extra nodal involvement is an important clinical observation. These cases are usually DLBCL, GCB type, and infrequently have concurrent MYC/BCL2/BCL6 rearrangement. Our study suggests that BCL with high-level MYC amp may have an aggressive disease course regardless of MYC, BCL2 and BCL6 gene rearrangement status. A larger series is necessary to further understand the clinical significance of high-level MYC amp in BCL.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.